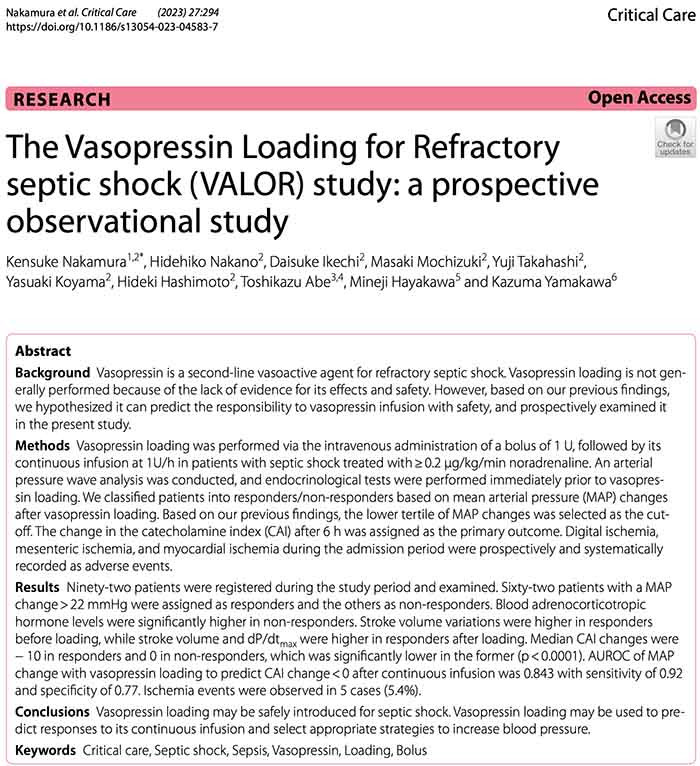
vasopressin challenge: this group evaluated 1U bolus of vasopressin to evaluate patient responsiveness
I love this for a few reasons:
[1] allows vaso to have rapid onset (rather than taking 30-60 min to build up)
[2] we can get a sense of whether the vaso is helping
🧵 1/5 #EMIMCC
I love this for a few reasons:
[1] allows vaso to have rapid onset (rather than taking 30-60 min to build up)
[2] we can get a sense of whether the vaso is helping
🧵 1/5 #EMIMCC
Comments
Thank you for quoting this trial!
this feels true - my philosophy has always been that if pressors don't increase BP they aren't helping (eg they're squashing CO)
(limitation: retrospective, may just be selecting less ill pts)
🧵#2/5
vaso causes venoconstriction & ⬆️ preload
high SVV suggests a preload-responsive heart
so preload responsiveness = venoconstriction responsiveness 🤯
(NOT necessarily an indication to give more fluid 😁)
🧵#3/5
this hasn't been part of my usual practice but, I think it makes sense (half-life of ~15-20 minutes, so you need a bolus to see any immediate effect)
(bonus points: who would do this thru a peripheral IV? 🫣)
🧵#4/5
Can’t be more dead than already dead 😅🫣
- they increase afterload
- heart can't tolerate afterload so CO *decreases*
- MAP = (CO)(SVR) is *unchanged*
so failure of a pressor to increase MAP may suggest that it's squashing the CO & not helping the patient
🧵#5/5
It’s true, but if I am on 1mcg/kg/min of norad then maybe we need to consider that it’s not an SVR problem!
Over 5 mins? How was this actually done?